THE Modern Outpatient
A Person-Centred Vision of Care for People Living with Multiple Long-Term Conditions for The Modern Outpatient Programme
Background
In this project, we responded to a challenge set by The Modern Outpatient Programme at the Scottish Government, to identify opportunities to innovate care for people living with multiple long-term conditions.
In Scotland, it is estimated that 47 per cent of the adult population have at least one long term condition and the number of people who live with multiple and complex conditions is growing. Currently our specialist care is delivered in hospitals, with each condition treated separately. This way of organising care requires people living with multiple conditions to attend many different appointments, which impacts on their lives and can be very tiring, and also represents an inefficient use of NHS resources. This project asked the questions:
The project was undertaken between August 2017 and February 2018, with the purpose of informing the ongoing and future work of The Modern Outpatient Programme.
PROJECT VIDEO
Video credit: Louise Mather, No Middle Name, 2018
Project Aims
The aim of the project was to develop a person-centred vision for the future of outpatient care for people living with multiple long-term conditions. The objectives were:
1) To understand the current challenge, specifically:
a) The challenges of living with multiple long-term conditions and the kinds of support people value;
b) The challenges health professionals experience in supporting people living with multiple long-term conditions within the current health and care system;
c) The challenges of innovating in outpatient care.
2) To generate ideas for new ways of working to support people living with multiple long-term conditions:
a) To understand how people living with multiple long-term conditions would like to be supported in the future;
b) To support NHS staff to co-design new person-centred models of care to meet the needs and aspirations of people living with multiple long-term conditions.
3) To distill the insights and ideas generated into a roadmap for the development of person-centred models of care, supported by new digital tools.
Methodology
Credit: Tara French, 2017
Public Engagement
Two pop-up public engagement events took place in the outpatient reception areas of Raigmore hospital in Inverness and Dr Gray’s hospital in Elgin. These sessions aimed to start a conversation with the public about what they value about outpatient services and gather ideas to improve their experience. The pop-up materials included sketches of design concepts that built on insights from DHI phase one research, alongside the provocation ‘What if…? Share your ideas for improving outpatient care’. Design concepts for the pop-up were generated during an internal workshop, which involved designer researchers from the Future Health and Wellbeing Research Group at GSA Innovation School responding to a series of briefs focused on reimagining the outpatient waiting room. Conversations with the public were recorded on panels as sketches and on post-its, which were used as inspiration materials in subsequent workshops.
Interviews
Credit: Louise Mather, No Middle Name, 2017
We interviewed four people living with multiple long-term conditions. In each interview, we worked together to make a visual map of their experience, recording how they currently manage their conditions as part of their daily life. We looked back to their experience of diagnosis and learning about their condition, and looked forward to understand their aspirations, and what future care they would value. Experiences of living with conditions such as diabetes, angina, depression, epilepsy, Crohn’s disease and arthritis were explored. The interview maps were used as the central inspiration for our co-design workshops.
Three further interviews were conducted with a consultant cardiologist, a programme manager for long-term conditions and a member of the Modern Outpatient team. In addition the design researcher observed a focus group session with staff from cardiology services across Scotland. These activities aimed to understand the current challenges in innovating outpatient services.
Credit: Paul Campbell 2017
Workshops
Three workshops with NHS staff took place in Glasgow, Forres and Edinburgh. These sessions brought together consultants, GPs, nurses, allied health professionals, telehealth experts and managers from six NHS regions, to consider the current experience of services for people living with multiple long-term conditions. We shared the stories of the people we interviewed using the visual maps. The participants were asked to place a chosen individual at the centre, designing care around their needs and aspirations.
Policy Review
In parallel with these activities, the DHI Research and Knowledge Management Team have undertaken a collation, review and summation of key documents relating to outpatient services in Scotland. Ten key documents were identified and summarised, with key themes identified. A connecting thread of these documents was the drive towards ‘person-centred care’; the use of this term has been reviewed across the documents to consider commonalities and differences in how this term is defined, what it means in practice for people living with long-term conditions and health and care professionals, and how it can be measured. This review is presented in an accompanying report, “Defining Person-Centred Care” which can be downloaded at the bottom of the page. The key points from this review have been translated into a visual summary of person-centred care (see Figure 3 on page 5).
findings
Introduction
During our pop-up public engagement we learned that people highly value the health professionals and assistants who listen and understand their needs as an individual. People told us about incredible doctors, nurses and teams taking great care of themselves or their loved ones. We also learned about the frustrations of parking near to the hospital, and the need for more practical information before an appointment.
From our interviews with people living with multiple long-term conditions, we understood the importance of a person's experience when receiving a diagnosis. This can impact on how people feel about their condition, how they engage with health professionals and the time it takes for them to accept, learn and manage their condition. The early stages can be an anxious time, and there is an opportunity to improve the information shared about what they can expect from both the condition and the health service.
We also learned that people rarely have conversations with health and care professionals that consider the impact of their multiple conditions and discuss their health and wellbeing in an integrated way. These types of conversations are vital in understanding how to self manage, and in supporting people to live well with their conditions.
One of the most insightful moments from the process was seeing the transformative power of the real stories captured in the interview maps. Interview participants generously shared their ‘health stories’ through the maps: NHS staff told us that having this level of insight into the person’s past experiences and aspirations for living well with their condition is hugely valuable in understanding how to design their care.
Through the co-design workshop we were able to place these real people at the centre of the service, and through this NHS staff identified many opportunities to innovate care.
current state mapping
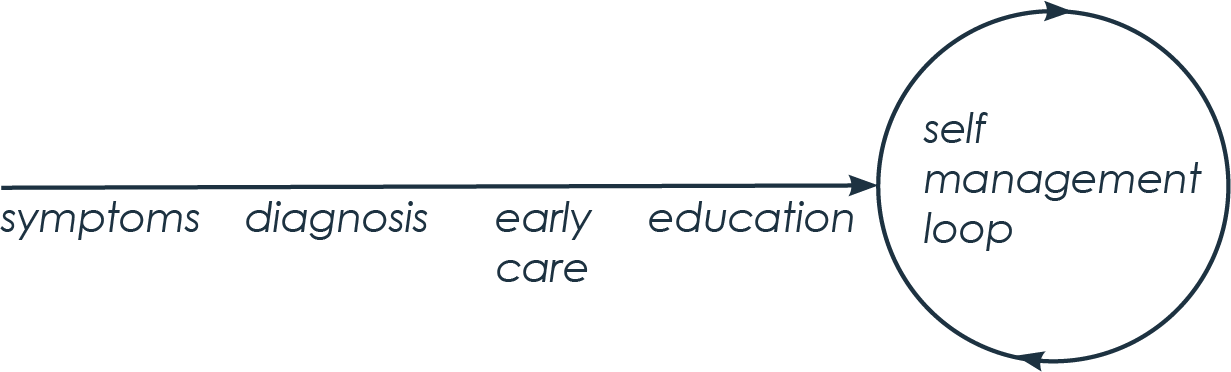
Representation of the journey of a person living with a long-term condition
Credit: Gemma Teal 2018
The insights about the current challenge and ideas for the future are mapped onto a simple representation of the journey of a person living with a long-term condition: the straight line representing their path from first symptoms through diagnosis, clinical management and education; a circle representing their ongoing experience of self management.
MAP 1: The current experience of care from the perspective of people living with multiple long-term conditions
Credit: Gemma Teal 2018
MAP 2: The current experience of care from the perspective of NHS staff
Credit: Gemma Teal 2018
person centred job description
Reflecting on the aspirations for future care people shared during the interviews, we generated a ‘person-centred job description’, specifying the activities, expertise and skills people were seeking from their health and care professionals. We shared this with NHS staff at our co-design workshops, and tasked them with designing the ideal future care team to fulfil the aspirations of people living with multiple long-term conditions.
Credit: Gemma Teal 2018
future state mapping
This map presents the new ideas generated through co-design activities plotted along the trajectory of care. Existing service development and innovations highlighted by participants were also included in this map.
MAP 3: Mapping ideas across the outpatient journey
Credit: Gemma Teal 2018
The overarching goal of increasing the value of appointments but decreasing the frequency was shared among people living with multiple long-term conditions, NHS staff and policy makers. To this end, many of the ideas relate to improving the quality of interactions with health professionals through resources and ways of working that centre the conversation on the goals of the person.
Many of these new ways of working rely on improved access to person-centred information and communication, that can be shared throughout the health and care team. Complementary links are drawn to the Backpack Personal Data Store project, currently at the proof of concept stage of development.
future vision
Credit: Gemma Teal 2018
design concepts
Credit: Gemma Teal 2018
Next Steps
The design team are currently exploring how the design concepts generated through this project can be taken forward in the DHI 'Future of Care' project. Essential to this process will be the meaningful involvement of people living with long-term conditions and NHS and social care staff to ensure the resulting resources meet the needs of the different users and stakeholders. Early and iterative prototyping will be used to translate the design concepts into tangible forms that can be tested and refined by the intended users to understand how they might support self management, service delivery and positive experiences of care.
Meanwhile, we are continuing to explore the outputs of the Backpack project and are developing prototypes and demonstrations of new concepts for care enabled by person-owned data. We are also working to translate The Modern Outpatient project outputs into the DHI Demonstration Environment to allow us to communicate the future vision using 'after' stories to bring the future vision of care to life and show the impact this would have on the lives of people living with multiple long-term conditions.
Acknowledgements
We would like to thank all of our interview participants for giving up their valuable time and for generously sharing their stories to inspire service redesign.
We would also like to thank The Health and Social Care Alliance (The ALLIANCE) for supporting recruitment of interview participants, and for members of The Modern Outpatient Programme team for supporting recruitment of NHS staff for co-design workshops.
Finally, many thanks to managers at Raigmore Hospital and Dr. Gray’s Hospital for permitting and facilitating our pop-up public engagement sessions in their busy outpatients foyers, and to all the citizens and staff who engaged with us to share their views.
download the report
Download the final report of this project, or the summary report:
Final Report: Print friendly A4
Final Report: Screen friendly A3
Further Information
For more information about this project please contact:
Gemma Teal, G.Teal@gsa.ac.uk
Cate Green, C.Green@gsa.ac.uk